Weighed at Birth is the Number of Children Discrete or Continuous
Birth Weight
From Embryology
Jump to:navigation, search
| Embryology - 20 Oct 2022 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
| العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose.
Introduction
There are a variety of prenatal techniques for estimating approximate birth weight that are relevant for preterm, term and prolonged pregnancy. Ultrasound two- and three-dimensional scanning methods are the basis of most current techniques. There are also standard autopsy weight curves that have been developed from second and third trimester fetal and also neonatal autopsy. Low birth weight is accurately defined as a statistical indicator for development. High birthweight definition on the other hand varies in the literature and between countries with a lower cut-off above 4000 gm or 4500 gm.
At birth, infants are generally weighed as soon as possible and may also be monitored during the neonatal period. In Australia, the average birthweight for all babies born: (1991) 3,350 grams, (2004 3,370 grams and (2015)[1] 3,327 grams. Also in 2015 6.5% (19,852) of liveborn babies were of low birthweight.[1]
- Links: ultrasound | DOHAD | maternal diabetes | macrosomia
| Birth Links: birth | Lecture - Birth | caesarean | preterm birth | birth weight | macrosomia | Birth Statistics | Australian Birth Data | Developmental Origins of Health and Disease (DOHAD) | Neonatal Diagnosis | Apgar test | Guthrie test | neonatal | stillbirth and perinatal death | ICD-10 Perinatal Period | Category:Birth | ||
|
Some Recent Findings
- New Australian Birthweight Centiles [2] "All singleton births in Australia of 23-42 completed weeks' gestation and with spontaneous onset of labour, 2004-2013. Births initiated by obstetric intervention were excluded to minimise the influence of decisions to deliver small for gestational age babies before term. Current birthweight centile charts probably underestimate the incidence of intra-uterine growth restriction because obstetric interventions for delivering pre-term small for gestational age babies depress the curves at earlier gestational ages. Our curves circumvent this problem by excluding intervention-initiated births; they also incorporate more recent population data. These updated centile curves could facilitate more accurate diagnosis of small for gestational age babies in Australia."
- Fetal brain development in small-for-gestational age (SGA) fetuses and normal controls [3] "Objective To assess whether fetal brain structures routinely measured during the second and third trimester ultrasound scans, particularly the width of the cavum septi pellucidi (CSP), differ between fetuses small for gestational age (SGA), fetuses very small for gestational age (VSGA) and normal controls. Methods In this retrospective study, we examined standard ultrasound measurements of 116 VSGA, 131 SGA fetuses and 136 normal controls including the head circumference (HC), transversal diameter of the cerebellum (TCD), the sizes of the lateral ventricle (LV) and the cisterna magna (CM) from the second and third trimester ultrasound scans extracted from a clinical database. We measured the CSP in these archived ultrasound scans. The HC/CSP, HC/LV, HC/CM and HC/TCD ratios were calculated as relative values independent of the fetal size. Results The HC/CSP ratio differed notably between the controls and each of the other groups (VSGA P = 0.018 and SGA P = 0.017). No notable difference in the HC/CSP ratio between the VSGA and SGA groups could be found (P = 0.960). The HC/LV, HC/CM and HC/TCD ratios were similar in all the three groups. Conclusion Relative to HC, the CSP is larger in VSGA and SGA fetuses than in normal controls. However, there is no notable difference between VSGA and SGA fetuses, which might be an indicator for abnormal brain development in this group."
- Diagnosing Small for Gestational Age during second trimester routine screening: Early sonographic cluesFatihoglu E & Aydin S. (2020). Diagnosing Small for Gestational Age during second trimester routine screening: Early sonographic clues. Taiwan J Obstet Gynecol , 59, 287-292. PMID: 32127152 DOI. "Small for gestational age (SGA) is generally defined as birth weight being at or below the 10th percentile. Children with SGA have a higher risk for complications. There is a need for early predictors, as the accurate diagnosis rate is only 50%. In the current study, we aimed to evaluate diagnostic performance of ultrasound (US)/color Doppler ultrasound (CDUS) parameters (umbilical vein-UV, right portal vein-RPV diameter/flow rate, and portal sinus-PS diameter) examined at 20-22 gestational week as SGA diagnostic factors. CONCLUSION: UV, RPV, and PS diameters can be earlier predictors for SGA diagnosis. Routinely evaluation of these parameters during second trimester screening can increase SGA diagnosis rates and serve for early diagnose."
- Impact of biometric measurement error on identification of small- and large-for-gestational-age fetuses [4] OBJECTIVES: First, to obtain measurement-error models for biometric measurements of fetal abdominal circumference (AC), head circumference (HC) and femur length (FL), and, second, to examine the impact of biometric measurement error on sonographic estimated fetal weight (EFW) and its effect on the prediction of small- (SGA) and large- (LGA) for-gestational-age fetuses with EFW < 10th and > 90th percentile, respectively. CONCLUSIONS: Measurement error in fetal biometry causes substantial error in EFW, resulting in misclassification of SGA and LGA fetuses. The extent to which improvement can be achieved through effective quality assurance remains to be seen but, as a first step, it is important for practitioners to understand how biometric measurement error impacts the prediction of SGA and LGA fetuses."
| More recent papers |
|---|
| This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Birth Weight | Small for Gestational Age | Large for Gestational Age | Low Birth Weight | Very Low Birth Weight | Extremely Low Birth Weight | High Birth Weight Birth Weight Z-score | |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table. See also the Discussion Page for other references listed by year and References on this current page.
|
Birth Weight Classifications
The primary causes of VLBW are premature birth (born <37 weeks gestation, and often <30 weeks) and intrauterine growth restriction (IUGR), usually due to problems with placenta, maternal health, or to birth defects. Many VLBW babies with IUGR are preterm and thus are both physically small and physiologically immature.
| | no colour | ||||||||||
| Birth weight (grams) | less 500 | 500 – 999 | 1,000 – 1,499 | 1,500 – 1,999 | 2,000 – 2,499 | 2,500 – 2,999 | 3,000 – 3,499 | 3,500 – 3,999 | 4,000 – 4,499 | 4,500 – 4,999 | 5,000 or more |
| Classification | | | | | | ||||||
Extremely Low Birth Weight
- Less than 500 grams (1 lb 1 oz or less)
- 500 – 999 grams (1 lb 2 oz – 2 lb 3 oz)
Very Low Birth Weight
- 1,000 – 1,499 grams (2 lb 4 oz – 3 lb 4 oz)
Low Birth Weight
- 1,500–1,999 grams (3 lb 5 oz – 4 lb 6 oz)
- 2,000–2,499 grams (4 lb 7 oz – 5 lb 8 oz)
Normal Birth Weight
- 2,500–2,999 grams (5 lb 9 oz – 6 lb 9 oz)
- 3,000–3,499 grams (6 lb 10 oz – 7 lb 11 oz)
- 3,500–3,999 grams (7 lb 12 oz – 8 lb 13 oz)
High Birth Weight
- 4,000–4,499 grams (8 lb 14 oz – 9 lb 14 oz)
- 4,500–4,999 grams (9 lb 15 oz – 11 lb 0 oz)
- 5,000 grams or more (11 lb 1 oz or more)
- see also macrosomia
Weight Conversions
| Extremely Low Birth Weight | Very Low Birth Weight | Low Birth Weight | Normal Birth Weight | High Birth Weight (macrosomia) |
|---|---|---|---|---|
|
|
|
|
|
No Background Version
| Birth weight (grams) | less 500 | 500 – 999 | 1,000 – 1,499 | 1,500 – 1,999 | 2,000 – 2,499 | 2,500 – 2,999 | 3,000 – 3,499 | 3,500 – 3,999 | 4,000 – 4,499 | 4,500 – 4,999 | 5,000 or more |
| Classification | | | | | | ||||||
Small for Gestational Age
Small for gestational age (SGA) is a term used for infants as having a birth weight more than 2 standard deviations (SD) below the mean or less than the 10th percentile for the gestational age (GA). WHO birthweight definitions are low birthweight as less than 2,500 grams, very low birthweight is less than 1,500 grams and extremely low birthweight: less than 1,000 grams. Growth restriction can be symmetrical (slow development with limited brain growth) or asymmetrical (head circumference and length are preserved and brain growth is relatively spared).
- Symmetric SGA (Weight, head circumference and length all below the 10th percentile) can be due to chromosomal abnormalities, intrauterine infection, severe placental insufficiency and or a constitutionally small infant.
- Asymmetric SGA (Weight below the 10th percentile) can be due to interference with placental function and or interference with maternal health in 3rd trimester.
There are a large number of known relationships between low birth weight and both maternal and fatal abnormalities, a few examples are shown below.
Z-score
The birth weight Z-score is a predictor of adverse neonatal outcome in severe placental insufficiencies.[14] For an individual birth weight, a z-score of -1 is one standard deviation below the mean birth weight of the cohort.
The Z-score classification system can be used to compare a child or a group of children to the reference population.
The Z-score (SD-score) = (observed value - median value of the reference population) / standard deviation value of reference population.
- Z-score scale is linear - therefore a fixed interval of Z-scores has a fixed height difference in cm, or weight difference in kg, for all children of the same age.
- Z-scores are sex-independent - allows evaluation of children's growth status by combining sex and age groups.
- Z-scores allow statistical calculations - such as means, standard deviations, and standard error to classify a population's growth status.
The Z-score classification system can also be used for population-based assessments, for example to monitor nutritional status malnutrition, health and within nutrition centers.
The z-score differences (Zdiff) uses standard deviation scores to analyze changes in growth for a particular observation period.
- Links:WHO
Fetal Gastroschisis
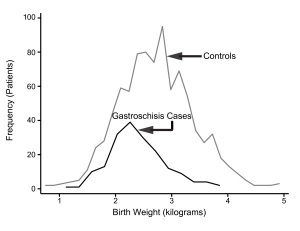
Gastroschisis Birth Weight Graph
Gastroschisis patients are commonly small for gestational age (SGA, birth weight < 10th centile). Frequency line graphs of the birth weight distribution.[15]
The abnormality is usually situated to the right of the umbilicus and abdominal contents, mainly gastrointestinal, are found outside the anterior body wall. Can occur in isolation and also in association with other gastrointestinal anomalies (intestinal atresia, perforation, necrosis or volvulus). Defects in other organ systems have been reported in up to 35% of children.
Maternal Elevated Testosterone
Maternal elevated testosterone levels is associated with low birth weight in humans. Hyperandrogenism associated with polycystic ovarian syndrome (PCOS) and pre-eclampsia have a higher prevalence of small-for-gestational age newborns. A rat model study suggests that maternal testosterone does not cross the placenta, to directly suppress fetal growth, but affects nutrient delivery to the fetus by down-regulating specific amino acid transporter activity.[16]
High Altitude
Altitude affects growth patterns measured in a a recent Peruvian study of 63,620 healthy infants born at low (150 m) and high (3000-4400 m) altitude were compared.[17] They found that in the third trimester "Mean and median birth weight differences between those born at low and high altitudes reached statistical significance after 35 and 33 weeks, respectively."
Canada
Definition: Live births with a birth weight of 4,500 grams or more, expressed as a percentage of all live births with known birth weight.
High birth weight can result in complications for the infant and mother during birth and may be associated with an increased risk of diabetes.
- Links: Canada Statistics | Statistics Canada, Vital Statistics, Birth Database.
Australia - Indigenous
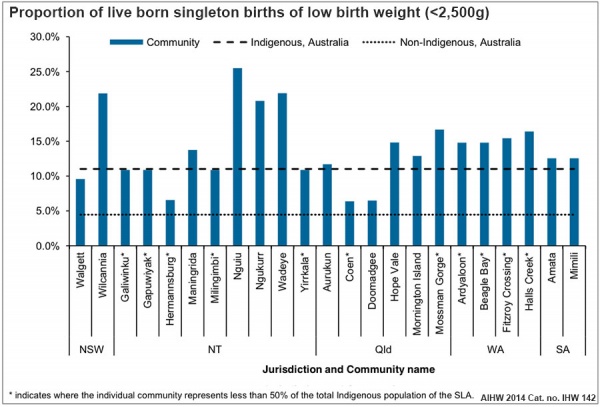
Australian low birth weight (2008–2009)[18]
Data in graphs below from AIHW 2014 Report, Birthweight of babies born to Indigenous mothers.[10]
- Links: Australian Statistics | Preterm Birth | SmokingBirth weight reference percentiles for Chinese===
China
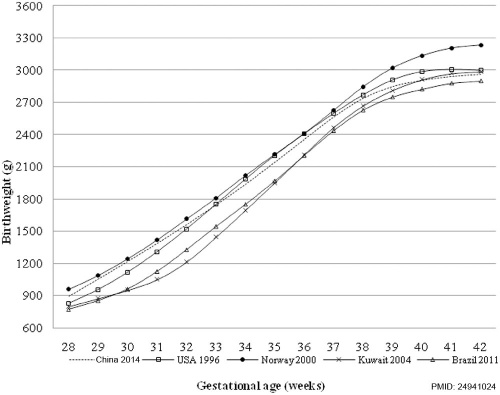
Birth weight reference percentiles for Chinese[12] "There have been moderate increases in birth weight percentiles for Chinese infants of both sexes and most gestational ages since 1980s, suggesting the importance of utilizing an updated national reference for both clinical and research purposes."
- Links: China Statistics
References
- ↑ 1.0 1.1 Australian Institute of Health and Welfare 2017. Australia's mothers and babies 2015—in brief. Perinatal statistics series no. 33. Cat no. PER 91. Canberra: AIHW.
- ↑ Joseph FA, Hyett JA, Schluter PJ, McLennan A, Gordon A, Chambers GM, Hilder L, Choi SK & de Vries B. (2020). New Australian birthweight centiles. Med. J. Aust. , , . PMID: 32608051 DOI.
- ↑ Jacob E, Braun J, Oelmeier K, Köster HA, Möllers M, Falkenberg M, Klockenbusch W, Schmitz R & Hammer K. (2020). Fetal brain development in small-for-gestational age (SGA) fetuses and normal controls. J Perinat Med , , . PMID: 32126016 DOI.
- ↑ Wright D, Wright A, Smith E & Nicolaides KH. (2020). Impact of biometric measurement error on identification of small- and large-for-gestational-age fetuses. Ultrasound Obstet Gynecol , 55, 170-176. PMID: 31682299 DOI.
- ↑ Freedman AA, Hogue CJ, Marsit CJ, Rajakumar A, Smith AK, Goldenberg RL, Dudley DJ, Saade GR, Silver RM, Gibbins KJ, Stoll BJ, Bukowski R & Drews-Botsch C. (2019). Associations Between the Features of Gross Placental Morphology and Birthweight. Pediatr. Dev. Pathol. , 22, 194-204. PMID: 30012074 DOI.
- ↑ Takemoto R, Anami A & Koga H. (2018). Relationship between birth weight to placental weight ratio and major congenital anomalies in Japan. PLoS ONE , 13, e0206002. PMID: 30346975 DOI.
- ↑ Salcedo-Bellido I, Martínez-Galiano JM, Olmedo-Requena R, Mozas-Moreno J, Bueno-Cavanillas A, Jimenez-Moleon JJ & Delgado-Rodríguez M. (2017). Association between Vitamin Intake during Pregnancy and Risk of Small for Gestational Age. Nutrients , 9, . PMID: 29168736 DOI.
- ↑ Paltiel O, Tikellis G, Linet M, Golding J, Lemeshow S, Phillips G, Lamb K, Stoltenberg C, Håberg SE, Strøm M, Granstrøm C, Northstone K, Klebanoff M, Ponsonby AL, Milne E, Pedersen M, Kogevinas M, Ha E & Dwyer T. (2015). Birthweight and Childhood Cancer: Preliminary Findings from the International Childhood Cancer Cohort Consortium (I4C). Paediatr Perinat Epidemiol , 29, 335-45. PMID: 25989709 DOI.
- ↑ Upadhyay K, Pourcyrous M, Dhanireddy R & Talati AJ. (2015). Outcomes of neonates with birth weight⩽500 g: a 20-year experience. J Perinatol , 35, 768-72. PMID: 25950920 DOI.
- ↑ 10.0 10.1 AIHW 2014. Birthweight of babies born to Indigenous mothers. Cat. no. IHW 138. Canberra: AIHW. Viewed 5 August 2014 http://www.aihw.gov.au/publication-detail/?id=60129548202
- ↑ Li Z, Wang YA, Ledger W & Sullivan EA. (2014). Birthweight percentiles by gestational age for births following assisted reproductive technology in Australia and New Zealand, 2002-2010. Hum. Reprod. , 29, 1787-800. PMID: 24908671 DOI.
- ↑ 12.0 12.1 Ye J, Zhang L, Chen Y, Fang F, Luo Z & Zhang J. (2014). Searching for the definition of macrosomia through an outcome-based approach. PLoS ONE , 9, e100192. PMID: 24941024 DOI.
- ↑ Adams-Chapman I, Hansen NI, Shankaran S, Bell EF, Boghossian NS, Murray JC, Laptook AR, Walsh MC, Carlo WA, Sánchez PJ, Van Meurs KP, Das A, Hale EC, Newman NS, Ball MB, Higgins RD & Stoll BJ. (2013). Ten-year review of major birth defects in VLBW infants. Pediatrics , 132, 49-61. PMID: 23733791 DOI.
- ↑ da Silva FC, de Sá RA, de Carvalho PR & Lopes LM. (2007). Doppler and birth weight Z score: predictors for adverse neonatal outcome in severe fetal compromise. Cardiovasc Ultrasound , 5, 15. PMID: 17374167 DOI.
- ↑ Payne NR, Simonton SC, Olsen S, Arnesen MA & Pfleghaar KM. (2011). Growth restriction in gastroschisis: quantification of its severity and exploration of a placental cause. BMC Pediatr , 11, 90. PMID: 22004141 DOI.
- ↑ Sathishkumar K, Elkins R, Chinnathambi V, Gao H, Hankins GD & Yallampalli C. (2011). Prenatal testosterone-induced fetal growth restriction is associated with down-regulation of rat placental amino acid transport. Reprod. Biol. Endocrinol. , 9, 110. PMID: 21812961 DOI.
- ↑ Gonzales GF & Tapia V. (2009). Birth weight charts for gestational age in 63,620 healthy infants born in Peruvian public hospitals at low and at high altitude. Acta Paediatr. , 98, 454-8. PMID: 19038011 DOI.
- ↑ AIHW 2014. Health indicators for Remote Service Delivery communities: a summary report. Cat. no. IHW 142. Canberra: AIHW. Viewed 5 November 2014 http://www.aihw.gov.au/publication-detail/?id=60129548650.
Reviews
Articles
Hemming K, Hutton JL & Bonellie S. (2009). A comparison of customized and population-based birth-weight standards: the influence of gestational age. Eur. J. Obstet. Gynecol. Reprod. Biol. , 146, 41-5. PMID: 19581044 DOI.
Search Pubmed
Search Pubmed: Low Birth Weight | small for gestational age
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- METoER (Australia) Birth—birth weight, code N
- CDC (USA) Pediatric Nutrition Surveillance System - Birthweight
- WHO Low Birthweight (2004) PDF
| Birth Terms | ||
|---|---|---|
| ||
|
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2022, October 20) Embryology Birth Weight. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Birth_Weight
-
- What Links Here?
- © Dr Mark Hill 2022, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G
goodridgebetteramer.blogspot.com
Source: https://embryology.med.unsw.edu.au/embryology/index.php/Birth_Weight

Enregistrer un commentaire for "Weighed at Birth is the Number of Children Discrete or Continuous"